#Cervical insufficiency
Explore tagged Tumblr posts
Text
Grieving Levi: Leaning into Perfect Placement
I feel like time is moving rapidly. Today is Levi’s due date, April 1st, 2024. Did we really go through all of that in December and it’s already April? Goodness. I really believe that in order to tell you of all the miraculous things God was and is doing through Levi’s brief time here, I need to start from the beginning. While Levi was our 3rd pregnancy loss in 4 years, I feel like I need to…
View On WordPress
#cervical insufficiency#church#church family#church placement#early stillbirth#Faith#God#grief#grief and loss#Hope#incompetent cervix#Jesus#loss#miscarriage#pregnancy after loss#pregnancy loss#stillbirth
0 notes
Text

Explore the meaning of high-risk pregnancy. Understand the factors and care needed for a healthy pregnancy journey. Learn about High Risk Pregnancy.
Do Read: https://www.drshubhragoyal.com/welcome/blogs/introduction-to-high-risk-pregnancy--what-does-it-mean
#High Risk Pregnancy#Pregnancy with heart disease#Rh incompatibility#Oligohydramnios#Uterine fibroids pregnancy#Pregestational diabetes#Cervical insufficiency#Pregnancy after 35#Recurrent miscarriages#Intrauterine growth retardation#Placental abruption#VBAC risks (Vaginal Birth After Cesarean)#Perinatal infections#Pregnancy-induced hypertension#Chronic kidney disease pregnancy#Antiphospholipid syndrome pregnancy#Congenital anomalies risk
1 note
·
View note
Text
Pregnancy complications can include conditions such as anemia, cholestasis of pregnancy, gestational diabetes, preeclampsia, ectopic pregnancy, placenta previa, placental abruption, preterm labor, hyperemesis gravidarum, miscarriage, stillbirth, infections, Rh incompatibility, gestational hypertension, and cervical insufficiency. And this isn’t even all of it. It’s beyond disrespectful to suggest a woman would go through all of that just to wait nine months to abort. No one endures the physical, emotional, and mental toll of pregnancy for nine months only to make that decision at the end.
26 notes
·
View notes
Text
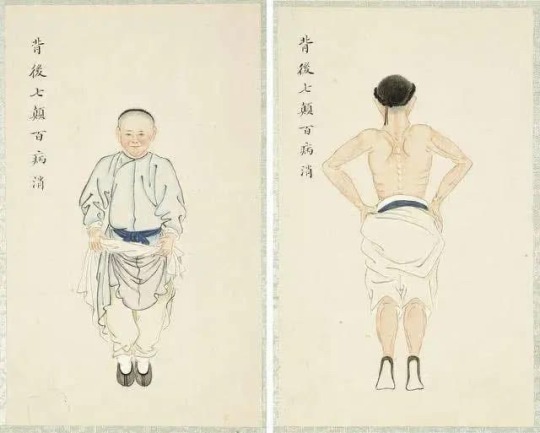
Standing on tiptoes: an action that has been passed down for 800 years. Do it seven times a day for one minute to replenish kidney qi, treat back pain, and prevent stroke (Figure 2)
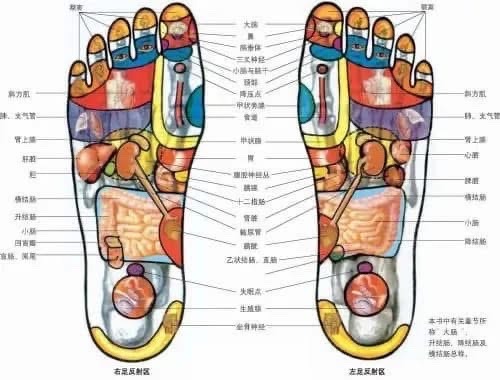
Another reason is that the subcutaneous fat layer of the feet is thin, and if you pull up the epidermis, there is almost nothing but bones underneath, so it is easier for external pathogens such as wind, cold, and dampness to invade the body.
The blood supply is slightly insufficient compared to the legs and arms, so cold evil can easily invade here and gradually accumulate, spreading upward and inward to other parts of the body.
Only by warming up and protecting your feet can the cold evil have difficulty invading the body.
Standing on tiptoes: an action that has been passed down for 800 years. Do it seven times a day for one minute to replenish kidney qi, treat back pain, and prevent stroke (Figure 3)
The Book of Changes says: "To repeat its course every seven days is the way of Heaven. " The Records of the Grand Historian records: "The number of yang is seven. " This is the natural rhythm of the movement of celestial bodies and yin and yang.
The reason why the feet need to be shaken seven times in the saying “Shake the back seven times to get rid of all diseases” is probably a reflection of the cultural connotation of the infinite reciprocating and rhythm of life represented by the number “seven”.
Five benefits of regular foot shaking
1. Antidepressant
Depression is caused by the inability of Yang Qi to reach the brain to nourish the brain marrow, resulting in poor circulation of Qi and blood in the brain and the blocking of the clear orifices by turbid Yin.
Tapping the heels can simultaneously stimulate the bladder meridian and the three yin meridians of the foot, including the kidney meridian, spleen meridian, and liver meridian. The yin and yang energy of the three yin meridians of the foot are sufficient, which can promote the flow of yang energy upwards, allowing more qi and blood to reach the head and face.
2. Replenish kidney qi
People with weak kidney qi and insufficient kidney yang often have symptoms such as fear of cold, cold and painful heels, and edema of the lower limbs. Shaking the heels can supplement the kidney qi and promote its function of promoting yang qi, and the effect is obvious.
3. Treat low back pain
Due to the invasion of wind, cold and dampness into the bladder meridian, the circulation of qi and blood is not smooth, and pain occurs when the circulation is blocked.
Therefore, the heel-tapping method, which can stimulate the bladder meridian, can also prevent and treat low back pain, cervical spondylosis, occipital headache, etc.
4. Prevent stroke
Traditional Chinese medicine believes that all strokes are symptoms of yin-excess and yang-deficiency caused by the decline of true yang, and cerebral hemorrhage is a symptom of yang rushing upward due to "yin-excess and yang-deficiency".
Stimulating the heels of the feet can not only stimulate the circulation of qi and blood in the brain, but also lead the floating yang downward through the bladder meridian and kidney meridian to the soles of the feet.
5. Treat urinary problems
In Western medicine, difficulty in urination is a prostate disease, which is often seen in prostate hypertrophy, prostatitis, etc. From the perspective of traditional Chinese medicine, it is caused by unfavorable bladder gasification.
Stimulating the heels is a little trick to treat prostate disease.

14 notes
·
View notes
Text
by Nicolas Hulscher, MPH
The study by Dr. James Thorp et al, titled, Are COVID-19 Vaccines in Pregnancy as Safe and Effective as the Medical Industrial Complex Claim? Part I, was just published after successful peer review in the journal Science, Public Health Policy and the Law:
Introduction: In Part I of this three-part series, we report a retrospective, population-based cohort study assessing rates of adverse events (AEs) in pregnancy after COVID-19 vaccines compared to the same AEs after influenza vaccines and after all other vaccines. Methods: Data were collected from the U.S. Centers for Disease Control and Prevention (CDC) and the U.S. Food and Drug Administration (FDA). The CDC/FDA Vaccine Adverse Event Reporting System (VAERS) database was queried from January 1, 1990 to April 26, 2024, for adverse events (AEs) involving pregnancy complications following COVID-19 vaccination. The time-period included 412 months for all vaccines except COVID-19 vaccines, having been used for only 40 of the 412 months (December 1, 2020 to April 26, 2024). Proportional reporting ratios (PRR) by time compared AEs after COVID-19 vaccination to those after influenza vaccination, and after all other vaccine products administered to pregnant women. In cases in which the PRR was not applicable, Chi-square analysis and Fisher’s exact tests were used according to CDC/FDA guidance. CDC/FDA stipulate a safety concern if a PRR is ≥ 2 or if a Chi-square is ≥ 4. Results: The CDC/FDA’s safety signals were breached for all 37 AEs following COVID-19 vaccination in pregnancy including miscarriage, chromosomal abnormalities, fetal malformations, cervical insufficiency, fetal arrhythmia, hemorrhage in pregnancy, premature labor/delivery, preeclampsia, preterm rupture of membranes, placental abnormalities, fetal growth restriction, stillbirth, newborn asphyxia and newborn death. All p values were ≤ 0.001 with the majority being <0.000001. Conclusions: We found unacceptably high breaches in safety signals for 37 AEs after COVID-19 vaccination in pregnant women. An immediate global moratorium on COVID-19 vaccination during pregnancy is warranted. The United States government, medical organizations, hospitals, and pharmaceutical companies have misled and/or deceived the public regarding the safety of COVID-19 vaccination in pregnancy. The promotion of the COVID-19 vaccines in pregnancy by The American College of Obstetricians and Gynecologists (ACOG), The American Board of Obstetrics & Gynecology (ABOG), and The Society for Maternal Fetal Medicine (SMFM) must cease immediately.
5 notes
·
View notes
Text
We're recovering.
A month on gynecology, my favorite rotation, helped. Better hours, got to participate in a couple of hysterectomies (doing about 1/3 as an R2 isn't bad, and even got a couple vag hysts under my belt), went to the gym more frequently, spent time with MIGS attendings and made some decisions/organized plans to move me towards MIGS applications next year, deepened some friendships.
I'm on MFM now, which I'm neutral towards. I hated it last block, but this block I'm mentally doing better. I'm motivated to read (I've gone pretty in depth on cervical insufficiency and incidental short cervical lengths, aortopathies, anticoagulation in pregnancy, and syphilis). I don't like early hours and long MFM rounding, but I do like reading! I do like learning! I've enjoyed listening to my attendings diffuse hard situations (a 30 weeker with ICP demanding delivery) and bad news (a new diagnosis at term of fetal hypoplastic left heart syndrome). Nothing I want to do in my career, but it's at list enriching to experience.
I'm making small steps with research: submitted my first IRB for my residency project, made my second round of manuscript revisions for for my medical school project, trying to get an away research rotation to bolster my CV for MIGS. I'm slowly putting project pieces together for my advocacy extracurriculars: organizing an ACOG event, building a webinar for the new OB/GYN application. I got back into my favorite organization app (Omnifocus) and am trying to keep on top of all these tasks and my bills and the miscellaneous texts I need to send. I feel like maybe things are coming together.
I am, however, struggling to balance learning and free time. I come home and read, read, read for work and then don't get a lot of free time and get overwhelmed and burn out. A symptom of my new ADHD diagnosis? Perhaps. Perhaps not. Doesn't matter, I still need to figure out how to cope. It's Sunday and I'm working on MFM and MFM-adjacent things until 5 PM and then I'll try to relax. One of my best friends visited this weekend which was the only reason I wasn't working unnecessarily hard on Saturday.
I go to nights next. 5 weeks of it, which will be the longest I've ever done. I like nights in the sense that at this point in the year I'll hopefully be first pick for arrest cesareans, and my job will be keeping an eye on antepartum and covering the gyne service/consults. Ante is usually somewhat quiet overnight and I like gyne. But 5 weeks? 14-16 h shifts? No sunlight, free time? It will be rough. At least I have 4/5 weekends. And I'll be working on this new medication trial. Which is a mess in and of itself.
But, again, we're healing. And I'm working really, really hard to make sure I'm set up for success as I become a senior next year, especially with being the Saturday 24 h call chief taking care of every single service! It's terrifying but also exciting, because while the growth is going to be fucking painful, I'll be so well-prepared for my true chief year coming out of it.
So uhhhh. We'll see. Life is ups and downs. Finally, I'm on a long-overdue upswing.
6 notes
·
View notes
Text
In the midst of an unseasonal California heat wave last late spring, Nathaniel DeNicola, an obstetrician-gynecologist at Hoag Hospital in Newport Beach, had an unusual case on his hands: A patient who had been carrying a perfectly healthy pregnancy for 32 weeks was going into early labor. It didn’t make sense; nevertheless, the baby was coming. The patient’s waters had broken, the baby’s heartbeat was dropping fast, and the child was in the breech position. The mother had an emergency C-section. After spending a couple of weeks in the neonatal intensive care unit, the baby was allowed to go home.
After the scramble to deliver the baby, DeNicola searched for reasons that might explain the premature arrival. Sometimes there are obvious causes for the early rupturing of membranes, like a chlamydia infection or a condition called cervical insufficiency, in which the cervix starts to dilate on its own. But those explanations didn’t fit DeNicola’s patient. Struggling, he settled on a different explanation: the searing heat. “I can’t prove that that was because of extreme heat; it’s very tough to assign that,” he says. But from his research, he knew that heat can trigger preterm births. And in his 12 years as a clinician, he has often seen more obstetric emergency visits during heatwaves.
Doctors have known for some time that certain groups of people, like the elderly and children, are particularly vulnerable to heatwaves. But in recent years, a new population has come into focus: pregnant people and their unborn babies. As the world warms up, there is a growing corpus of evidence that the heat is interfering with pregnancy, perturbing the delicate fetus in the womb, with the potential for serious complications.
And it’s plenty hot now. July 3 was the hottest day ever recorded globally. July was declared the hottest month on record. California’s Death Valley recently reached 128 degrees Fahrenheit—just two degrees short of a record for the entire planet. In Phoenix, Arizona, the daytime temperature hasn’t dipped below 110 degrees Fahrenheit in almost a month. In parts of the world, such as Iran, the heat index is teetering toward the threshold of what the human body can tolerate. Swathes of Europe are on fire.
Understanding the effect of extreme heat on pregnancies will require a major shift. Due to ethical concerns, pregnant people have typically been excluded from studies of the effects of heat on physiology. (A recent paper drily pointed out that far more research has been done on the effects of heat stress on livestock “due to its economic importance.”) It means that much of what we know comes from animal studies.
So far, there are many theories, but not many firm conclusions. Animal studies have shown that heat can provoke an increase in the secretion of oxytocin, a key hormone involved in labor, which may also explain the phenomenon in humans. It could be that extreme heat triggers the premature rupture of membranes, leading to a too-early birth. Or it could be that heat strain causes the release of inflammatory proteins, prompting preterm labor. Maybe it’s dehydration caused by the heat, causing the release of prostaglandins, lipids that will trigger contractions, and these contractions can be so intense that the body goes into early labor.
In pregnant people, we know that the body alters the way it regulates its temperature to accommodate for increased body size and the metabolic toil required to grow a baby. This, in turn, limits the body’s capacity to dissipate heat. So when it’s super hot, a pregnant person is perhaps less equipped to deal with the heat. Another theory is that when a pregnant person is experiencing heat stress, the body releases heat-shock proteins, which could trigger physiological reactions that are harmful to the baby and its bearer.
A few papers have tried to pinpoint how heat affects the development of human babies, notably a 2022 study that followed 92 pregnant farmers working in The Gambia in West Africa. Led by Ana Bonell, a research fellow at the London School of Hygiene & Tropical Medicine, the team wanted to figure out how doing agricultural labor out in the heat was affecting their pregnancies. Bonell knew that heat stress can trigger the release of cortisol, which could hinder blood flow to the placenta. So her team decided to measure stress, both on the mother and the fetus. Alarmingly, they saw that for every 1 degree Celsius increase, there was a 17 percent increase in fetal stress—defined as abnormally high heart rate or slower blood flow through the umbilical cord. Overall, they concluded that heat strain on the mother translated into strain on the fetus.
Bonell felt it was important to be doing the research in a region likely to face some of the worst tolls of a heating world, where the typical escapes—say, retreating to an air-conditioned building—aren’t available to all. “There’s a massive inequality and climate justice agenda that goes with any research around climate change,” she says. “West Africa is one of the most vulnerable to the impacts of climate change. It just felt right, really.”
Strain on the fetus can have serious consequences. Multiple studies have found that even small increases in ambient temperature can increase the risk of preterm birth: A study from California found that for every 5.6 degrees Celsius increase in ambient temperature exposure, the risk of a preterm birth increased by 8.6 percent. Another analysis also found that the risk of preterm birth increased as temperatures went up.
Several studies have also found significant links between heat exposure and low birth weight. A 2022 study conducted in Massachusetts found that higher ambient temperature resulted in smaller babies. One reason why, the paper proposes, is that perhaps the induced heat-shock proteins mess up normal protein synthesis, which may wreak havoc with the development of the fetus’s organs.
For some babies, the heat can prove fatal. Another recent analysis led by Bonell reviewed the link between heat exposure and stillbirths: One study from Western Australia found that the risk of stillbirth increased by 41 percent if the mother was exposed to moderate heat stress—around 32 degrees Celsius—in the last two weeks of pregnancy.
And hot weather may affect a baby’s development in other ways: A 2021 analysis found a higher incidence of anomalies, such as cardiac defects, spina bifida, or cleft lip, at higher temperatures. A 2019 study took existing research that linked heat exposure to congenital heart defects and extrapolated how many such cases we can expect in the coming years: The authors estimated that over an 11-year period, an additional 7,000 babies will be born with congenital heart defects in the eight US states they studied. According to Bonell, there’s also early evidence from animals that heat stress may be triggering epigenetic changes linked to long-term adult chronic diseases such as heart disease and diabetes.
And in the United States, any potential harm to a fetus brings with it other concerns. Pregnant people, more than ever in a post-Roe world, are at risk of criminalization for behavior that may harm the fetus, particularly in states that recognize fetal personhood, which grants legal rights to a fetus from conception. “You might live in a state that criminalizes your adverse birth outcome because you took a walk when it was hot, or you were working outdoors when the temperatures were too high,” says Adelle Dora Monteblanco, an assistant professor of public health at Pacific University in Oregon.
As the research linking extreme heat to pregnancy complications piles up, public health bodies, including the World Health Organization and UNICEF, have started to take notice and include pregnant people and their unborn babies in warnings during extreme heat—although some, like the United Kingdom, are still leaving pregnant people out. While including pregnant people in public health messaging is important, doctors also need to do more to keep patients fully informed on how to stay safe. “We know enough to act,” says DeNicola. “While we don’t have perfect solutions, we do have counseling we can give.” He knows to tell his patients to drink more water, and try to access any kind of cooling, if they have the means. If air-conditioning isn’t an option at home, people should look for cooling centers, or shopping malls, movie theaters, or libraries.
Research has shown that more targeted advice is still a necessity. A 2022 paper concluded that current guidance for pregnant people with regard to heat exposure is “sparse, inconsistent, and not evidence based.” Big questions remain, like at what stage in the pregnancy is the mother and fetus most at risk, or at what temperature conditions shift from risky to dangerous.
Yet there are limits to simply giving out advice. As the world heats up, pregnant people and their babies will continue to be vulnerable to these risks—particularly people from low-income households and people of color. Bonell points out that what people really need is practical help or the tools to help themselves. “You need some other solutions that aren’t just about education,” she says.
11 notes
·
View notes
Text
Update on Ro is apparently she has symptoms of cervical insufficiency which after Sage would make sense….if that’s the case they’re advising termination because it will only cause more problems for Violet….- Harry
2 notes
·
View notes
Note
on a scale of one to ten how dumb was it
A 9.
If it had been an actual doctor lecturing, it would've been the stupidest thing I've ever heard on the basis they should've known better.
As it was, it was a former Physician's Assistant (PA), who still should've know better.
I'll likely be banned from the noontime resident grand rounds for my outburst, which is sad because they have the best lunches.
Readmore for the topic of abortion, specifically ectopic pregnancy.
The topic for grand rounds was Holistic Approaches to Medicine and the Importance of Spiritual Well-Being, which the speaker who was a former PA decided to go into a pro-life rant mid-lecture.
At this point, if you're a medical student or a resident, you've probably made your decision on abortion. So, fine.
But what came out of his mouth afterwards was so stupid and dangerous, regardless of whatever side of the debate you take, that I thought I hallucinated his comments. And only by looking at the host of the grand rounds - an attending-level doctor like myself - staring in horror at the speaker made me realize that what he said was real.
Essentially the speaker was stating as fact that ectopic pregnancies, a pregnancy outside the uterus, are no longer a valid excuse to get an abortion, because women have survived and delivered such pregnancies to full-term.
----
Okay first off, some basics. Let's talk about where the fetus ends up in a normal pregnancy. It should be within the uterus, specifically the uterine cavity.
Anywhere else is known as an ectopic pregnancy. Too low, and you have a cervical ectopic which will usually spontaneously abort in the first trimester. But for this post, we'll talk about the ectopic pregnancies that implant in the fallopian tube/around that region (most common type of ectopic) or the abdomen (the most likely chance of fetus surviving full-term).
Tubal ectopic pregnancy occurs approximately 95% of all ectopic pregnancies. The egg implants inside the tiny Fallopian tube that connects your ovary to the uterus, and the embryo grows. And because it grows, it can rupture the tube that is in - and can potentially cause the mother to bleed to death.
Abdominal ectopic pregnancy occurs approximately 1% of ectopic pregnancies. The abdomen's problem in that the fetus attaches somewhere that it's not meant to - like an organ or your abdominal lining. The reason why such an ectopic pregnancies can very rarely carry to full-term is because of the available space - there's nothing confining it. However, make no mistake that it's still an ectopic. These ectopics can still result in catastrophic hemorrhage such as through perforating an organ with its implantation and kill the mother.
Now there are very rare cases of ectopic pregnancies coming to full term, mostly abdominal ectopics for the reason stated above. Most fetuses will die because of insufficient blood supply or implantation. Others who make it often have major birth defects because of the above and the usually low amniotic fluid levels (the fluid the baby floats in). The mothers that carry out an ectopic pregnancy to term and survive with a healthy baby are lucky - like winning the lottery sort of lucky. Simple as that.
The usual outcomes of an untreated ectopic pregnancy is either spontaneous abortion or it grows and ruptures wherever it's located, risking the life of the mother. Ectopic pregnancies are the leading cause of the mother dying in the 1st trimester of pregnancy and account for 5-10% of all pregnancy related deaths. It is a big deal.
--
The notion that the speaker was using these incredibly rare cases of survival and using them to justify not having abortions for ectopic pregnancies is appalling - and presenting it as fact in a teaching institution even more so.
I stated in exact words that "that is the most absurd thing I've ever heard."
And when he tried to smugly double down by quoting papers about these rare case reports like they were the norm - and continued to argue that we should do watchful waiting and only intervene if there's problems, I figuratively slammed the door shut in his face.
Even putting aside the fact that ectopic pregnancies have almost virtually no chance to make it to viability, when these things rupture, you might not even get a chance to go to the hospital and just bleed to death. Pain is often one of the first signs that an ectopic pregnancy is there in the first place - that's the moment to intervene. When you have worsening pain past that, that could already mean it ruptured.
He then tried to argue that everyone deserves a chance. I asked him if everyone includes the mother, which made him bristle.
At that point, the veneer of friendliness fell away, and he demanded I leave the auditorium for interfering with his lecture. I told him in no uncertain terms that I was staying, and if he's going to try and pass off the rare as common, I am going to call him out every single time.
He ended up being the one walking out, calling me shameful and disrespectful and with no respect for life.
I let him have his parting comments.
The residents and I spent the next 3 minutes in silence before the other attending doctor dismissed them all - and just looked at me as if wanting to say something before shaking his head.
5 notes
·
View notes
Text
Introduction to High-Risk Pregnancy- What Does It Mean

Pregnancy can indeed be a joyous time, but it can also be overwhelming and stressful. Expectant mothers need to take care of themselves and their unborn babies. However, for some women, their pregnancy is considered high-risk.What is a high-risk pregnancy? It means the mother has an increased chance of experiencing complications during pregnancy, labor, delivery, and even after birth. Understanding this can help expectant mothers plan accordingly.Factors that contribute to high-risk pregnancy can vary from woman to woman. Some common factors include age, weight, medical history, and lifestyle choices. Awareness of these factors can help women make informed choices during this crucial time.So, let's dive deeper and understand what medical conditions can cause high-risk pregnancies and how to reduce the risks.So, let's get started!High Risk Pregnancy: Quick Overview!Pregnancy is a unique and beautiful journey, but it has challenges. As the name suggests, a high-risk pregnancy involves a higher likelihood of complications than a typical pregnancy. These complications can arise due to various factors, such as pre-existing medical conditions, age, or a history of pregnancy-related issues. Let's explore some common aspects that can categorize a pregnancy as high-risk.Factors that Contribute to High-Risk Pregnancy!Age is one of the factors that contribute to high-risk pregnancy. Women older than 35 are at increased risk. Other factors include Pre-existing medical conditions, Multiple pregnancies, substance abuse, and more.According to the insights, high-risk pregnancies accounted for 11.5% of all pregnancies, whereas moderate pregnancies accounted for 21.6%. 33.1% of pregnancies overall had high or medium risk.Pregnancy brings a lot of physical changes in a woman's body, making it more vulnerable to certain medical conditions. Some medical conditions that can cause high-risk pregnancy include hypertension, gestational diabetes, and preeclampsia.1. HypertensionHypertension or high blood pressure is a condition in which the mother's blood pressure is higher than the ideal range. Hypertension can lead to complications such as preterm labor, low birth weight...2. Gestational DiabetesGestational diabetes is a condition that can really affects pregnant women who didn't have diabetes before pregnancy. It indeed leads to high blood sugar levels, which can indeed cause complications such as preterm labor, macrosomia or a giant baby, and respiratory distress syndrome.3. PreeclampsiaPreeclampsia is a condition that affects pregnant women after 20 weeks of gestation. It leads to high blood pressure and damage to organs like the kidneys and liver. Preeclampsia can cause complications such as preterm delivery, low birth weight, and long-term health problems for both the mother and the baby.
Continue Reading: https://www.drshubhragoyal.com/welcome/blogs/introduction-to-high-risk-pregnancy--what-does-it-mean
#High Risk Pregnancy#Pregnancy with heart disease#Rh incompatibility#Oligohydramnios#Uterine fibroids pregnancy#Pregestational diabetes#Cervical insufficiency#Pregnancy after 35#Recurrent miscarriages#Intrauterine growth retardation#Placental abruption#VBAC risks (Vaginal Birth After Cesarean)#Perinatal infections#Pregnancy-induced hypertension#Chronic kidney disease pregnancy#Antiphospholipid syndrome pregnancy#Congenital anomalies risk
1 note
·
View note
Text
Advanced Directive OB obstetrician (University of Memphis) Scan to open on Studocu Studocu is not sponsored or endorsed by any college or university Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Advanced Directives Exam 1 Summer 2022 1. Fetal circulation The 2 arteries carry deoxygenated blood from the fetus to the placenta and the umbilical vein carries oxygenated blood to the fetus carries (oxygenated) blood to the embryo 2. Determine obstetrical history using GTPALM (GTPALM) -- birth information • G--ravidity- # of pregnancies (including present one) • T—erm births- pregnancy from 37 – 42 weeks • P—reterm births- pregnancy from 20 – ending prior to 37 weeks • A--bortion- (spontaneous or elective) termination of pregnancy before fetus is viable (< 20 weeks or < 500 g) • L--iving- # currently alive • M-multiples-# of deliveries that had more than 1 infant delivered 3. Differentiate between presumptive, possible and probable signs of pregnancy ➔ Presumptive – subjective – mother’s experiences ➔ Probable – objective – signs seen by examiner, could be cervical conjunction ➔ Positive – objective – fetus seen or heart tones heard 4. Calculate date of birth (EDC, EDB or EDD) using Naegele’s Rule Naegele’s Rulea. 1st day of LMP - 3 months + 7 days OR b. 1st day of LMP +9months + 7days 5. Amniotic fluid: function & how to determine if ROM Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 ● Protects the fetus, temperature control, cushions the baby from bumps and injury; rupture of membrane is determined with nitrazine test for pH (Ruptured - amniotic fluid is alkaline BUT so are bloody show, insufficient amniotic fluid, and semen) Blue-green Blue gray Deep blue or test for ferning (done under microscope by doctor) 6. Function of the placenta-provides O2 and nutrients; removes waste from the babies blood 7. Fetal development: actions, sex, heart, quickening, response to extrauterine activity, lungs, liver 3 weeks- ■Heart starts beating & blood circulates 4 weeks- ■2- chamber forms a 4- chamber heart ■Respiratory system begins 5 weeks- ■Umbilical cord developed 8 weeks- ■Gender distinguishable 9 weeks- ■Fingers, toes, eyelids, nose, & jaw evident 12 weeks- ■Placenta complete ■Organ systems complete ■Thumb sucking ■Fetus urinates in amniotic fluid-11 weeks 16 weeks- ■Meconium in bowel 20 weeks- ■Hearing developing ■Quickening (Mom feels movement) Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 ■Lanugo covers the body ■Wake/sleep cycles evident 24 weeks- ■Circulation visible ■Rapid brain growth ■Hiccups ■Vernix caseosa is thick ■Lecithin (L) present 8. Using the menstrual cycle homework determine what part the following hormones are involved, what their action is and in what cycle or phase would you expect them to be activated: a. Estrogen-has a role in ovulation when the ovaries release an egg and thickens the lining of the uterus to prepare for pregnancy b. Progesterone-helps to regulate the cycle; if there is no fertilized egg, progesterone level drops and menstruation begins. (Pro- life). c. Follicle stimulating hormone-helps control the menstrual cycle and stimulates the growth of eggs in the ovaries; the levels change during the menstrual cycle; the highest levels happen right before an egg is released d. Gonadotropin releasing hormone-releasing hormone that releases folliclestimulating hormone and luteinizing hormone from the anterior pituitary; regulate ovarian function ➔ Ex: what phase and cycle is the Corpus luteum in? Luteal phase in the ovarian cycle 9. Physical changes regarding maternal heart, skin and feelings regarding pregnancy that would be considered normal during pregnancy Heart-increase in vascular volume, increase in RBCs, increased CO (BP does not increase) Skin:•Chloasma - Facial pigmentation •Linea nigra – a darkly pigmented line from the umbilicus to the pubic area •Striae gravidarum – stretch marks on trunk and thighs r/t stretching of connective tissue. •Palmar erythema – darker red palms r/t hyperemia Feelings-supine hypotension, SOB, N/V 10. Labs – Know normal for Hcg, Hgb, RPR (VDRL), RH factor and platelets for pregnant women Hcg ()-earliest biological marker for pregnancy Hct (34.6-43.8) Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Hgb (11.5-14.8) RPR -used to test for syphilis; A normal test result typically reveals that the blood does not contain any antibodies that are reactive to syphilis. RH factor() Platelets (150-400) normal to be higher have more going on 11. What would you teach a client that you suspect is being abused? ● A woman suspected of being emotionally or physically threatened or abused should be interviewed and examined in private. Most important, do you feel safe returning home? Assessment: ● 1. Regular screening of ALL women for history/risk of IPV ● 2. Most important - validate that they have been heard ● 3. Establish safety (at the moment and future) ● 4. Observe for injuries - old/new ● Partner asking questions versus patient ● 5. Associated health conditions warranting further assessment: HA, GI probs, chronic pain, arthritis, STIs, pelvic pain, substance abuse, depression, PTSD, suicide Education: ● 1. Abuse is a violation of rights ● 2. Facilitation of access to protective and legal services is first step 12. Why do teens have a delay in prenatal care ● Delayed entry into prenatal care can be the result of late recognition of pregnancy, denial of pregnancy, or confusion about the available services. Such delays in care leave an inadequate time before birth to attend to correctable health problems. Very young at risk for poor pregnancy outcomes. Higher risk for abuse and harder to enter the system don't have insurance, sacred attempting to hide pregnancy. 13. Potential complications in the first trimester: Hyperemesis gravidarum, UTI, contractions, DVT ● Hyperemesis gravidarum if persists longer than 1st trimester, nausea of pregnancy normally does not ● UTI correlated to preterm or pregnancy loss ● Hypercoagulable state more likely for DVTs (increased clotting factors) ● Contractions: braxton hicks thought to enhance blood flow; irregular and painless although some women complain that they are annoying 14. Weight gain during pregnancy Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Weight Gain (total = 25-35lbs) •2 to 4 lbs (1st trimester) •1 lb/week (2nd & 3rd trimester) 15. Using your presentation homework be able to determine presenting part Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Read the full article
0 notes
Text
youtube
Advancements in Laparoscopic Cerclage Surgery: Insights from Dr. B. B. Dash at WALS 2025 Conference
https://wals.world/
At the World Association of Laparoscopic Surgeons (WALS) 2025 Conference, esteemed gynecological surgeon Dr. B. B. Dash delivered an insightful presentation on Laparoscopic Cerclage Surgery, a revolutionary technique in managing cervical incompetence. His discussion provided an in-depth look at the indications, techniques, advantages, and future prospects of this minimally invasive approach to cervical cerclage.
Understanding Laparoscopic Cerclage Surgery Laparoscopic cerclage is a minimally invasive technique used to reinforce the cervix in women with recurrent pregnancy loss due to cervical insufficiency. Unlike traditional transvaginal cerclage, laparoscopic cerclage allows for precise suture placement, reducing complications and improving pregnancy outcomes.
Key Highlights from Dr. B. B. Dash’s Presentation
1. Indications for Laparoscopic Cerclage History of recurrent mid-trimester pregnancy loss Failed transvaginal cerclage procedures Congenital cervical anomalies Women undergoing assisted reproductive techniques (ART) with cervical incompetence
2. Surgical Technique and Innovations Dr. Dash elaborated on the step-by-step approach for laparoscopic cerclage, emphasizing: Preoperative assessment: Use of imaging techniques such as MRI and transvaginal ultrasound to evaluate cervical length and anatomy. Trocar placement and dissection: Precise port positioning to enhance visibility and maneuverability. Suture Placement: Use of non-absorbable polyester or polypropylene sutures at the level of the internal os, ensuring cervical reinforcement. Hemostasis and Closure: Application of minimal electrocautery to prevent tissue damage and ensure quick recovery.
3. Advantages of Laparoscopic Cerclage Over Traditional Methods Minimally invasive approach with smaller incisions and faster recovery. Higher success rates in preventing pregnancy loss compared to transvaginal cerclage. Better visualization of the cervix, allowing for precise placement of sutures. Lower risk of infection and postoperative complications.
Early placement advantage: The procedure can be performed before pregnancy, eliminating the risks associated with an emergent second-trimester cerclage. Clinical Outcomes and Research Findings Dr. Dash presented clinical data showcasing improved pregnancy retention rates with laparoscopic cerclage. Key findings include: Success rates exceeding 85% in preventing preterm birth. Reduced miscarriage rates in high-risk patients with cervical insufficiency. Shorter hospital stays and quicker return to normal activities. Minimal postoperative pain and complications.
Future Prospects and Innovations Dr. Dash also highlighted emerging advancements in laparoscopic cerclage, including: Robotic-assisted laparoscopic cerclage for enhanced precision and ergonomics. Integration of AI-based surgical navigation for optimized suture placement. Personalized patient selection protocols to improve outcomes in borderline cases. Conclusion The WAS 2025 Conference provided a platform to showcase the remarkable benefits of laparoscopic cerclage surgery in managing cervical incompetence.
Dr. B. B. Dash’s presentation reinforced the importance of this technique in preventing pregnancy loss and improving maternal-fetal outcomes. As laparoscopic and robotic advancements continue, laparoscopic cerclage is poised to become the gold standard in cervical insufficiency management. For further updates on minimally invasive surgical techniques and research, stay connected with the World Association of Laparoscopic Surgeons (WALS).
0 notes
Text
10 Essential Nursing Care Plans for Cervical Insufficiency: Comprehensive Guide & PDF Download
Cervical insufficiency, also known as an incompetent cervix, occurs when the cervix dilates without pain in the second trimester. Nurses detect this condition early and manage it to reduce risks of premature birth and pregnancy loss. This guide explains nursing care plans and provides a downloadable PDF for clinical practice and exam preparation. 1. Introduction Nurses play an essential role in…
0 notes
Text
"Maca: Nature’s Secret for Better Performance and Stamina"
A must-read for men | Introduction to the 4 major benefits of Maca. When is the best time to take it? Are there any side effects? What is Maca? 3 major categories Maca, native to the high-altitude mountainous areas of Peru in South America, is known as "Maca Ginseng" because of its rich root nutrients. With the widespread recognition of its nutritional value, maca is often used as an ingredient in health foods. According to research by the National Institutes of Health (NIH), the main nutrients in maca root include:
10.2% protein Maca - 59% carbohydrates
2.2% fat
8.5% fiber Maca Introduction Maca is also rich in a variety of unique and precious compounds, such as macaene and macaamide, which are significantly helpful for men's health. Maca can be divided into 13 types according to color. The most common ones on the market are black maca, red maca and yellow maca. Black Maca Introduction Black Maca is the rarest of all Maca varieties. Its macaene and macaamide content is relatively high, so the health care effect is relatively better, and the price is naturally more expensive. Introduction of Red Maca Red maca is rich in iron and calcium, and is especially suitable for women. Maca products designed for women on the market usually use red maca as the main ingredient. Yellow Maca Introduction Yellow Maca is the most common type, so it is less expensive and is used by most health food brands. 4 major benefits of Maca Maca's most well-known benefits are concentrated in men's health, including enhancing physical strength and improving athletic performance. Maca In addition, Maca is rich in nutrients, so it can also supplement nutrition and improve fatigue. Maca effect 1: Regulating physiological functions Maca contains a variety of proteins, carbohydrates and other nutrients, which help regulate physiological functions and maintain the normal functioning of the body. Maca Benefit 2: Helps with Athletic Performance Maca is rich in essential amino acids, such as leucine, arginine, phenylalanine and glutamate, which can help improve athletic performance. Maca effect 3: Improve fatigue and enhance physical strength Maca Maca is rich in vitamin C, vitamin A, vitamin B2, vitamin B6 and niacin, which helps to enhance physical strength and improve fatigue. Maca effect 4: nourishing and strengthening the body, men's health Maca's unique macaene and macaamide are beneficial for nourishing and strengthening the body, especially for men's health. Maca consumption time Maca is a health food rather than a medicine, so the effects are not immediately visible. However, long-term consumption can gradually adjust the physical condition. According to the literature, in terms of men's health, obvious effects can be seen after taking for 8 to 12 weeks. In general, like other health foods, maca needs to be consumed continuously to be effective. Temporary consumption has no obvious effect. 3 major side effects of Maca According to the literature, most studies have shown that maca is well tolerated by the human body, but a few have experienced transient side effects such as gastrointestinal discomfort, headache, and irritability. There is no need to worry about side effects of maca at normal doses, but if you experience any discomfort after taking it, you should stop taking it immediately and seek medical advice. Maca Consumption Taboo In addition to side effects, maca is not well studied in certain special groups, so the following groups should pay special attention:
Unprocessed maca contains ingredients that affect thyroid metabolism. If you have related diseases, you should consult a doctor.
Due to insufficient research, pregnant women, breastfeeding women and minors are advised to avoid consumption
Patients with hormonal disorders such as cervical cancer, ovarian cancer, breast cancer, etc. are advised to avoid eating
Maca is rich in vitamin K. People who take anticoagulant drugs should be aware that it may interfere with the efficacy of the drugs. Will eating maca Maca cause baldness? Won't. Although maca is thought to increase male hormones, there is no evidence that it changes hormone levels in the body and therefore does not cause baldness. When is the best time to take Maca? Since maca can enhance physical strength and maintain mental strength, it is generally recommended to consume maca during the day. As for whether to take it on an empty stomach or after a meal, it depends on the other ingredients in the maca product.
Eat on an empty stomach: Maca Arginine, probiotics
Take after meals: zinc, B complex, taurine Adjust according to your own situation. For example, it may be uncomfortable to take arginine on an empty stomach, so you can adjust the intake of maca to half an hour after a meal. How to better consume maca? Maca is rich in nutrients on its own, and its effects are even better when supplemented with other ingredients. Common combinations are as follows:
Refreshing, nutritional supplement: B complex, taurine
Men's Health: Arginine, Nitric Oxide
Maca for women's mature age maintenance: Vitamin C, calcium, iron
0 notes
Text
Miscarriage, preeclampsia, cervical insufficiency, chromosomal abnormalities, fetal malformations, premature birth, stillbirth, newborn asphyxia and newborn death were among the signals flagged by the peer-reviewed study, published last week.
by Brenda Baletti, Ph.D.
February 13, 2025
9 notes
·
View notes
Text
“USAID has pushed nearly half a billion dollars ($472.6m) through a secretive US government financed NGO, ‘Internews Network’ (IN), which has ‘worked with’ 4,291 media outlets, producing in one year 4,799 hours of broadcasts reaching up to 778 million people and ‘training’ over 9000 journalists (2023 figures).
An analysis of reports submitted to the Vaccine Adverse Event Reporting System (VAERS) found safety signals for 37 adverse events when COVID-19 vaccines were administered during pregnancy.
Miscarriage, preeclampsia, cervical insufficiency, chromosomal abnormalities, fetal malformations, premature birth, stillbirth, newborn asphyxia and newborn death were among the signals flagged by the study, published last week in the peer-reviewed journal Science, Public Health Policy and the Law.
A landmark lawsuit against Merck is underway in a Los Angeles courtroom, marking the company’s first jury trial over claims it misrepresented the safety of its highly profitable Gardasil HPV vaccine.
Newly declassified documents in the trial have revealed troubling details about Merck’s failure to conduct key safety tests.
Internal emails reveal that Merck knew its Gardasil vaccine was contaminated with HPV DNA fragments from the vaccine‘s manufacturing process and lobbied regulators to bypass testing requirements.
Uncovering residual DNA contamination
Concerns over Gardasil’s residual DNA contamination have persisted for over a decade.
In 2011, Dr. Sin Hang Lee, a pathologist with extensive experience in DNA analysis, discovered high levels of HPV DNA fragments in 16 Gardasil vials from several countries, including the U.S., New Zealand, Australia, Spain, Poland and France.
These DNA fragments, originating from the plasmid DNA used in vaccine production to code for the HPV virus’s L1 protein, are supposed to be removed during manufacturing.
0 notes